Share article:
How text messaging in healthcare improves patient outcomes

Even before the pandemic, text messaging platforms were revolutionising medical practices and practitioners engaged with patients and clients. Stemming from the simple appointment reminder, SMS text has helped patients and physicians communicate and engage in new and meaningful ways.
Let’s examine some considerations before we explore how text messages can effectively improve the overall healthcare experience.
Things to consider before adding text messaging solutions
Offer options
73% of customers globally prefer text messaging to other forms of communication. However, catering to all communication preferences is important when it comes to healthcare. Ensure you offer SMS as an option and retain consent before moving ahead.
Develop policies
Develop internal and external policies that cover privacy and compliance, as well as remit and scope.
Certain countries have local laws regarding the privacy and security of patients and their protected health information. For example, patient information passed through any communication means must be HIPAA compliant. This means, for example, it must go through secure text messaging routes. It is often on the onus of the business to ensure these rules are followed and adhered to. Contact our team of SMS experts if you have any questions.
Partner up
If you’re using other communication channels, consider how SMS can improve or strengthen current tactics. For example, if you are sending email appointment confirmations that are rarely read (20% open rate), consider adding a text message (98% open rate) in parallel.
Seek integrations
If you’re using a healthcare management platform, seek an integrated solution so that you can plug in text messaging directly. This will save you time switching between platforms and provide a whole host of other benefits.
RELATED: Peruse our entire integrations marketplace to see what we have on offer to make your life easier when integrating SMS!
Pick your provider
Pick your SMS messaging partner wisely! Ensure they understand and can advise you on compliance. They should also be able to support you with a product and service that will maintain security and privacy. When it comes to patient’s communications, this is essential!
6 ways you could start using SMS in your practice now
Appointment reminders
SMS appointment reminders can reduce no-shows on average 10-15%. Interestingly, when it comes to healthcare professionals or clinics, this can go up to 80%! Adopted widely by most healthcare clinics and practitioners, it is now expected by most patients that they will receive an SMS reminder before they attend an appointment. In fact, over-reliance on reminders may cause more no-shows for a business if they don’t adopt text alerts.
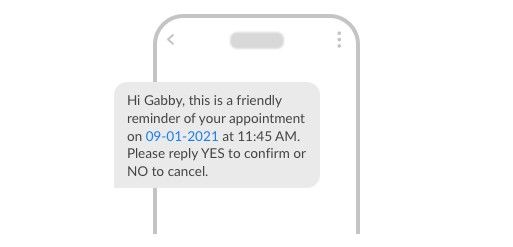
RELATED: Learn our 6 best practice tips for sending effective appointment reminder texts. They include advice on timing, frequency and what’s best to ensure cut through!
Emergency updates
During COVID, many clinics and healthcare organizations relied on text messages to communicate with patients quickly and in real-time. Given constantly changing conditions, physicians require solid communications that get read.
SMS has been long used in the emergency services spaces from alerts to potential bush fires to texting the police to having an emergency text service to serve the disabled.
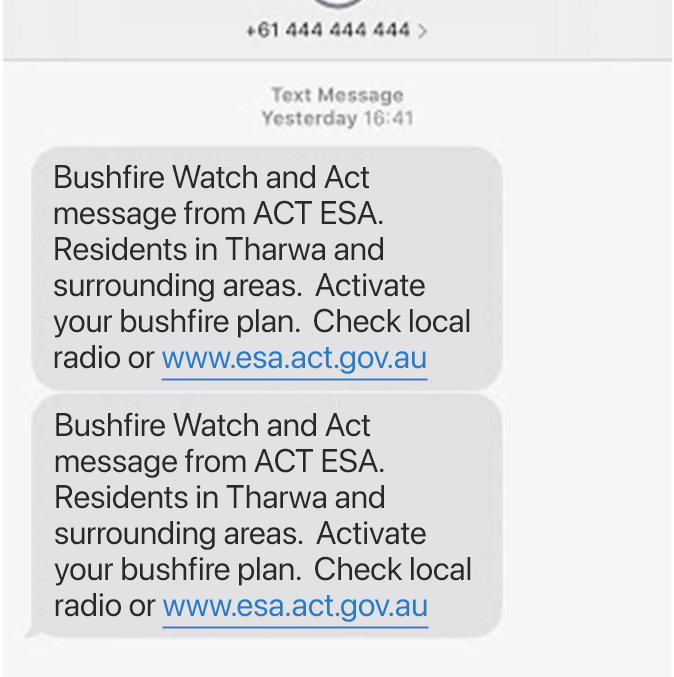
Practices may want to consider having additional emergency communication protocols in place. You could have automated text message announcements prepared for a wide range of potential eventualities, such as sudden or increased COVID infections.
Promoting health awareness and education
Some health providers are using text messaging as a preventative solution. Using text messaging to generate health awareness and create opportunities to support patients in taking care of their health in the long term, while also reducing unnecessary patient visits.
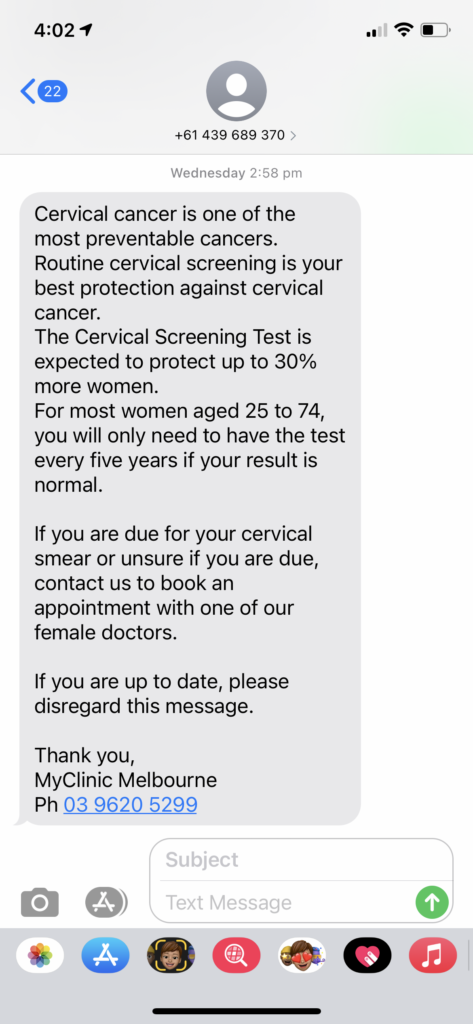
In one study, SMS supported the recall of a prostate intervention educational initiative among African American men – 65% wanted to receive more information via text even after the study had finished. In a Spain-based study, a high 68% of women attended breast screening exams if they were sent a text reminder 3 days beforehand.
SMS is more widely used as a tool for behavior change, especially with stagnant or inert audiences. We’re seeing this already in education where SMS is helping achieve better outcomes for students from poorer social-economic backgrounds and struggling with remote learning.
RELATED: Read about the 4 intriguing ways SMS is helping educators enhance remote learning.
Getting on the front foot with patients is a win-win situation for all. More direct and personalized engagement with patients will help maintain long-term relationships with a greater duty of care.
Keeping patients on track
Think outside the appointment box! Sending patients reminders can also help them stay on top of prescriptions or follow-up check-ins. Patients, as we know, are busy and forgetful. With automated scheduling provided by text message platforms, text messaging can become part of a larger end-to-end service experience for your patients – straight from their mobile devices!
Imagine the convenience of being able to reschedule your appointment, receive your prescriptions and get reminded about your next check-up. All from your mobile phone inbox!
Post or pre-medical check-ins
We’re seeing more service experience businesses take up check-ins with clients, whether they’re hair salons or personal trainers. Within the healthcare space, they can be even more effective as they can help physicians support clients between appointments.
However, they are often – and have been in the past – on the onus of the patient themselves.
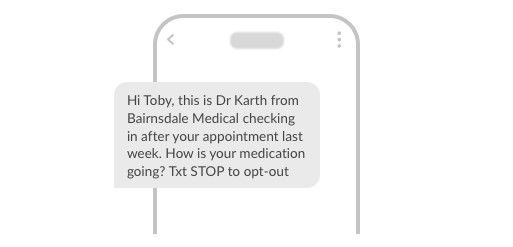
With patients who are demoralised, unable or forgetful; having physicians reach out can improve the customer experience 10x fold. Automated follow-ups need not be managed by busy practitioners. Instead, operational or office staff can deal with responses, and raise issues where serious feedback is given.
RELATED: To send automated check-ins or to enable 1:1 patient communications, turn on two-way texting! Learn more.
Increasing personalized patient engagement with feedback loops will only benefit your relationships and ensure improved patient care.
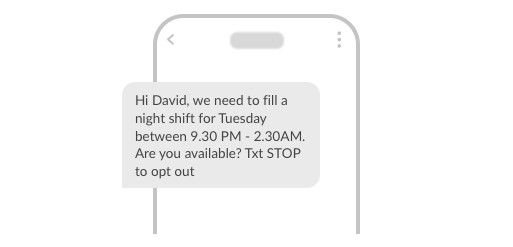
Internal scheduling and scheduling
Estia Healthcare dropped agency scheduling fees by 20% with SMS prompts to fill vacant shifts and roster reminders. One of the most under-utilised and overlooked use cases for messaging in healthcare is communications with your employees.
Internal reminders and prompts can be very useful. Sales agents receive one when a prospect needs to be followed up. They’re also used to remind employees about internal meetings. In fact, MessageMedia used text messaging to remind employees to update their personal contact information during COVID.
Our staff members are happy to receive texts notifying them of vacant shifts as it gives them an opportunity to earn extra money on top of their normal wage. And we’re happy, because using our own staff means we can ensure continuity of care, which is very important in aged care, and for our residents.
Jeremy Cassidy, Systems Manager, Estia Health Aged Care
For healthcare, it can prove even more important where it is almost essential for rostered medical workers to show up to their shifts where life and death might be on the line.
Final thoughts and further reading
The ways in which text messaging is used across the healthcare space keeps expanding. While we’ve only covered a few use cases, there are still many more out there that could change the way you help and improve patient outcomes and welfare. Do you know any we haven’t mentioned? Email us and let us know.
Make sure to also check out:
- How to improve your appointment reminders with these 6 best practice tips!
- 4 new ways healthcare practitioners can use SMS to innovate communications
- Webinar: Leverage SMS in healthcare to adapt to the new normal